 Your new post is loading...
 Your new post is loading...

|
Scooped by
nrip
|
The pandemic drove many patients to their primary care docs via video. And it worked. A telehealth expert (Dr. Peter Antall) explains how this shift could become a permanent hybrid with in-person care in an Interview with healthcareITNews Here is a summary from the interview. What is Virtual Primary Care Virtual primary care is allowing patients to see their primary care physician in person or virtually, depending on their needs. It combines the convenience of telehealth with the ability to strengthen recurring relationships with primary care physicians. It also can help provide a medical home for patients who have no primary care physician, either due to lack of access or lack of engagement. The emergence of virtual primary care stems from the recognition that the traditional primary care model doesn't work well for many patients. Access to care remains a major issue for many patients, due to geographical constraints and a growing shortage of primary care physicians, which has only been exacerbated by the pandemic. Do Patients Want it? Patients are receptive. A recent Amwell survey shows consumers want a virtual approach to primary care – - Most consumers (77%) would prefer to see their existing primary care provider via video.
- 25% of consumers are willing to switch providers to get it.
- 80% saying they would prefer to see the same primary care physician regularly via virtual care.
Can virtual primary care provide a simple, seamless care experience? How are patients supported throughout the care process? The best virtual primary care programs are well coordinated and enable a seamless care experience with the ability to transition patients between in-person and virtual care settings, and to various specialties or allied care providers as needed. In this way the care is holistic and the patient journey is clear and simple. Data sharing is an important part of creating a highly coordinated and seamless care experience. Records from all visits should be available to all providers on the telehealth platform across specialties and should be shared with the primary care physician in brick and mortar if one exists. This interoperability improves care and improves the referral and transition process. To ensure patients are supported, virtual primary care programs should include care coordination capabilities. For example, secure messaging between patients, healthcare professionals and administrative staff can help patients receive quick answers to their questions and ensure that all of their needs are met in a timely fashion, even after a visit has finished. Can virtual primary care help with population health? The flexibility of remote access makes it possible for providers to see patients' living conditions, evaluate social determinants of health, and respond in ways that make a deep impact on patients' lives. Providers also can leverage virtual primary care to evaluate medication adherence among patients with diabetes, hypertension and high cholesterol. When breakdowns in medication adherence are discovered, providers and support staff can work to engage patients in following their treatment plan more closely. This avoids complications that can occur when patients deviate from recommended treatment. Improvements in compliance and ongoing care can be accomplished through use of frequent brief touchpoints, care coordination, nudges and team-based care. Prompts and reminders can be used to reinforce the care plan. With capabilities such as these, virtual primary care positions providers and health plans not only to improve population health, but also to perform well under value-based models of care. More and more, it's clear that the future of care depends on hybrid models of care delivery such as this and I believe we've only just begun to scratch the surface of what's possible with virtual primary care and how it contributes to the continued transformation of healthcare. read the unedited article on the interview at https://www.healthcareitnews.com/news/will-virtual-primary-care-become-new-model-healthcare-delivery

|
Scooped by
nrip
|
For Yale New Haven Health System (YNHHS), a well-connected health IT infrastructure with a focus on communication and patient engagement tools has helped clinicians deliver a high quality patient experience. YNHHS’s focus on patient engagement tools, ranging from real-time surveys and telemedicine to patient portals and educational materials, has helped to reduce barriers to care access, improve satisfaction, and facilitate communication. Real-time surveys reward quality interactions One tool the health system uses is called Humm, a real-time patient satisfaction feedback survey deployed through a bedside tablet. Humm helps the care team gather data on room cleanliness, noise levels, and patient interactions with nurses and provider care teams. Using population health to improve care access Beyond understanding the patient and his or her needs at the point of care, Yale New Haven Health System is also dedicated to driving patient engagement to achieve population health management goals. more at http://patientengagementhit.com/news/health-it-communication-tools-key-for-quality-patient-experience

|
Scooped by
nrip
|
Virtual reality has been making headlines for its potential to transform the ways we interact with our environments. Breakthrough technologies like the Oculus Rift headset have made for incredibly lifelike experiences, notably in gaming and other forms of digital entertainment. Aside from its boom in the media sector, virtual reality has also emerged as an innovative tool in healthcare. Both virtual and augmented reality technologies are popping up in healthcare settings such as operating rooms, or being streamed to consumers via telehealth communications. In many cases, virtual reality has enabled medical professionals to execute care more safely and effectively. As virtual and augmented realities enter the mainstream, the technologies have become more accessible to the general consumer population. With a $15 price tag, Google Cardboard allows users to stretch physical limits with a smartphone — no extensive scientific knowledge required. That same philosophy is being applied to virtual reality in the healthcare industry, empowering patients to take charge of their health. Dr. Leslie Saxon, founder and executive director of the USC Center for Body Computing, is leading several initiatives to make virtual and mixed reality more patient friendly. The center’s Virtual Care Clinic system features an app that connects patients to medical expertise similar to what they would receive at the doctor’s office. The app displays Saxon’s image, guiding users through different courses of medical care. But patients using the app aren’t interacting with Saxon herself. Instead, they are following instructions issued by a virtual rendering of the doctor. Using a virtual human agent may seem like a detached method of doctor-patient communication, but Saxon believes it to be the exact opposite. With this kind of technology, she told Healthline, patients could get their questions answered in an environment free from judgment. They can access information on their own time and at their own pace.

|
Scooped by
nrip
|
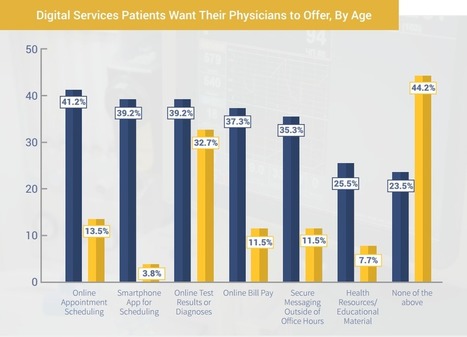
New patient engagement trends from TechnologyAdvice Research reveals digital engagement is a growing factor in how patients choose healthcare providers.
Quality of care has long been a primary factor in choosing a healthcare provider, but convenience and communication are also becoming key considerations for patients. Still, many physicians do not appear to be offering the digital engagement services that can meet those demands.
According to a new nationwide survey conducted by TechnologyAdvice Research, a majority of patients (60.8 percent) said digital services like online appointment scheduling and online bill pay are either “important” or “somewhat important” when choosing a physician. However, when asked what services their current physician provides, less than one-third of patients indicated they have access to either online bill pay, online appointment scheduling, or the ability to view test results and diagnoses online, which are the top three services that patients report wanting the most.
“Primary care physicians are reporting some of the highest rates of EHR adoption to comply with government regulations and to receive incentives from Meaningful Use, but a significantly lower number of patients claim to have access to these patient portal services,” said TechnologyAdvice Managing Editor Cameron Graham, who authored the survey. “The issue here may not be implementation of digital services, but instead a lack of patient awareness. If physicians are offering these in-demand digital services, a more proactive approach to promoting them is needed and could create an advantage in attracting and retaining patients.”
TAKEAWAYS
- If providers wish to gain an upper edge in attracting new patients (especially younger ones), and in retaining their existing patients, they should invest in a fully featured patient portal system. For many primary care physicians this should not be difficult. Most comprehensive EHRs include patient portal features, and dedicated patient portal vendors are making strides in integrating with third-party systems. In particular, prioritizing systems with intuitive online appointment scheduling, online bill pay functionality, and online test results could provide a significant draw for new patients.
- For practices that already have patient portal systems, they should dedicate resources to making sure their patient populations are informed of the existence of such services. They should also consider prominently featuring these services in their advertising and on their websites. When orienting new patients to their practice, providers need to have a plan for walking patients through the initial portal set-up requirements and making sure they understand the features available to them.
-For particularly tech-savvy practices, a dedicated smartphone app could help set them apart, and attract younger individuals.
more at http://hitconsultant.net/2015/01/16/should-physicians-tailor-patient-engagement-based-on-age/

|
Scooped by
nrip
|
Background: Mobile text messages are a widely recognized communication method in societies, as the global penetration of the technology approaches 100% worldwide. Systematic knowledge is still lacking on how the mobile telephone text messaging (short message service, SMS) has been used in health care services.
Objective: This study aims to review the literature on the use of mobile phone text message reminders in health care.
Conclusions: We can conclude that although SMS reminders are used with different patient groups in health care, SMS is less systematically studied with randomized controlled trial study design. Although the amount of evidence for SMS application recommendations is still limited, having 77% (46/60) of the studies showing improved outcomes may indicate its use in health care settings. However, more well-conducted SMS studies are still needed.

|
Scooped by
nrip
|
Though the industry has made outstanding progress in adopting EMRs, the practice of data acquisition from patients remains cloudy.
A recommendation from the HITSC Meaningful Use Workgroup would require practices with electronic health records (EHRs) to allow 10 percent of patients to report PGHD electronically.
If approved in meaningful use stage 3, the final stage of HealthIT.gov’s EHR incentive program, it could push hospitals to incorporate patient-generated data.
This requirement may seem like a relatively simple intervention, but the ramifications are quite significant. If clinical decision-making is made on the basis of data supplied by patients and documented in the EMR, how can clinicians be sure that such data is complete, correct and valid? And will clinicians like me learn to rely on it, or will we disregard it due to concerns about its validity or barriers to integrating it into care flow?
Furthermore, if a patient is in control of her health data entry, who is ultimately responsible for its completeness and accuracy — the patient or the clinician?
Incorporating biometric data into the EMR, an exciting prospect, is even more complex. Though clinicians are quite familiar with data entry from FDA-approved medical devices such as blood glucose meters, pacemakers and pulmonary function units, data from a myriad of consumer-driven health devices (Fitbit and others) will soon seek to flex their way into EMRs.
Patients clearly value these data; a recent Pew Research report noted that 60 percent of adults claim to track their exercise routine, weight or diet, meaning providers have some catch-up to do in order to meet patients halfway. Some health systems, such as Partners HealthCare, have already been experimenting with the incorporation of PGHD from remote devices into the EMR, and other institutions should follow.
Consumer health data devices are moving ahead at a staggering pace, and while the health care system can’t quite keep up, strategic planning should be happening now.
Despite the challenges, incorporating PGHD is a necessary evolutionary step for health care. Intelligently designed, well-executed systems that fully incorporate and display PGHD in a meaningful way will improve shared decision-making and enable patients as active care partners. Keen clinicians and patients will stay closely tuned to the numerous transformations to come.

|
Scooped by
nrip
|
You have attended and spoken at Doctors 2.0, why?
Kerri: The patient is so often talked about at medical conferences, but so rarely heard. I was honored that Denise Silber asked me to give one of the keynotes at Doctors 2.0 in 2013, because it gave me the chance to raise the voice of the patient, and to highlight how the diabetes online community works as a tide to raise all PWD (person with diabetes) boats.
Marie: The invitation to speak at Doctors 2.0 last year was a great honour for me. I already knew what an innovative and dynamic conference it would be, having followed along with it via Twitter for the previous two years. Not only did I get a chance to share my story at the conference, I also enjoyed meeting face- to-face those I had come to know online. I came away with new perspectives and ideas and stronger ties to many of my peers.
There are lots of medical apps available for smart phones and tablets, many of which are free or inexpensive. But how do you incorporate them into clinical practice?
The good news is you don’t have to invest in fancy equipment. If you’re asking about apps, you probably own a smart phone or tablet. Your patients who will benefit most from apps own the technology already, too. So the most efficient and effective way to start is to use the technology you have, and have learners use what they have.
Next step is to find the most appropriate resources. Do not start from “what apps are available?” That would not be patient-centered. Instead, ask: What conditions do my patients have? What do I teach about? What do my patients and their families need to learn? What questions do they have? What behaviors do they need help changing to optimize health?
There are 3 places apps might be used:
1. In the clinical encounter, as you explain something.
2. During a hospitalization, to engage the patient and family in the educational process.
3. At home, to provide information and support healthy behavior changes.
Read more: http://notimetoteach.com/2013/using-apps-to-enhance-patient-and-family-education/
Via Parag Vora
|

|
Scooped by
nrip
|
In this seventh installment in Healthcare IT News' feature series, Health IT Lessons Learned During the COVID-19 Era, A CIO, a CMIO and two IT directors offer readers what they've discovered since the pandemic response has reshaped health system priorities. They share what they've learned during the past year and discuss how they're applying these lessons to improve their organizations. The increased importance of data and analytics Overall, the COVID-19 pandemic has catapulted the importance of data analytics and data in general, For example, the data analytics team at Sanford Health designed an algorithm to sort and pull relevant data from the records of more than 100,000 patients who had been diagnosed with COVID-19, identifying those at highest risk of complications from the virus. More, more, more patient engagement For Averill of St. Luke's Regional Healthcare System, the impact of patient engagement using patient portal communication, virtual visits and digital appointment-scheduling provided a big lesson. They also expanded the amount of clinical information sent in real time to the portal since delivering in-person results wasn't possible. When telehealth is not up to par One major lesson Helio Health learned last year was that its telehealth presence was not up to par. On the other hand, the health system also learned that its teams could implement a telehealth presence fairly quickly. They had to pivot quickly to be certain their patients' critical care would not be interrupted by restrictions put in place as a result of COVID-19 Leveraging technology to further strategy Rollins of Freeman Health System said 2020 was a great year for health IT for many reasons. Many important initiatives were pushed forward and implemented in attempts to react to the ever-changing needs of our customers. Keeping strategies dynamic Another lesson Rollins has learned over the past year is that health IT and organizational strategies must leave room to adapt to the environment. Streamlined and efficient decision-making On another front, the pandemic has underscored the importance of having a structured mechanism and system in place for streamlined and efficient decision-making, Standardized processes and equipment Another lesson Helio Health has learned is the need for standardization of equipment and processes,. "The vast majority of our computers were desktop PCs," he noted. "With a grant from the FCC, we were able to standardize our outpatient facilities with Microsoft laptops, which allow us to work and provide support from anywhere. Users are able to come and go, from remote work to in-person work, easily. With a recent merger between Helio Health and two other organizations, much of the hardware from the other organizations was dissimilar to Helio Health's standards. read the details at https://www.healthcareitnews.com/news/it-execs-talk-new-strategies-analytics-patient-engagement-telehealth-and-more

|
Scooped by
nrip
|
More than 60% of smartphone users used their mobile device to search for information about a health condition, according to Pew Research Center. The analysts at eMarketer have forecast that pharma digital ad spending will rise to $2.55 billion by 2019.
This growing evolution in digital applications to monitor and improve health sets the foundation for new strategies in pharma marketing. Both physicians and patients are heavy users of mobile, and a new challenge arises when the industry shifts its focus to messaging targeting patients. Marketers now need to learn how to create a meaningful digital experience for patient-consumers.
The growth in mobile investment within the industry is real. For example, half of Takeda’s Web traffic last year came from smartphones and tablets, which is why the drug maker is optimizing mobile for both patients and physicians in its marketing campaigns. The real opportunities don’t lie in simply providing informational material — the app version of brochureware — but in finding simple ways to improve adherence and outcomes, When mHealth apps are paired with traditional treatments, this becomes possible. The industry needs to act on the opportunity to be in the pockets of its consumers read more at http://www.pharmavoice.com/article/2016-06-mobile-technology/

|
Scooped by
nrip
|
Although many people with serious diseases participate in online support communities, little research has investigated how participants elicit and provide social support on these sites.
This study by Yi-Chia Wang, Robert E Kraut, John M Levine Uses Computer-Aided Content Analysis to Examine the Dynamics of Online Social Support.
A high percentage of people with chronic or life-threatening diseases use online resources to obtain information about their condition and ways to cope with it. Although informational websites are the most popular, many people—especially cancer patients and survivors—participate in online health support communities.
A recent meta-analysis suggested that online support communities are effective in decreasing depression and increasing self-efficacy and quality of life. Although several clinical trials suggest that participation in Internet-based support communities improves emotional well-being, conclusions are ambiguous because most interventions have multiple components of which support group participation is only a part.
Moreover, research also shows that support interventions often do not provide the benefits they were designed to produce. Thus, much remains to be learned about when and why support is effective in online communities.
Conclusions of this study : Self-disclosure is effective in eliciting emotional support, whereas question asking is effective in eliciting informational support. Moreover, perceptions that people desire particular kinds of support influence the support they receive. Finally, the type of support people receive affects the likelihood of their staying in or leaving the group. These results demonstrate the utility of machine learning methods for investigating the dynamics of social support exchange in online support communities.

|
Scooped by
nrip
|
As practices look to integrate newer and hopefully advanced technologies to help them reduce readmission rates and improve outcomes, there is a lot to consider.
Buzzwords abound, like big data and coordinated care, but what those things actually mean vary largely from one place to the next.
ECRI Institute’s 2015 Top 10 Hospital C-Suite Watch List discusses a blend of novel, new, and emerging technologies that will demand attention and planning over the next 12 to 18 months, plus important issues and programs affecting care processes and delivery in 2015 and beyond.

|
Scooped by
nrip
|
While portal technology has been available in other industries for some years, access to health information and records via a secure login is only now becoming common place in healthcare by the end of the year.
Patient portal are excellent opportunities for providers to expand the way they engage with their patients. Here are a some best practices for using portals in your practice.
Increase Availability
Patients with full-time jobs don’t always have the flexibility to communicate or interact with you during your traditional office hours. By offering a robust patient portal system, ideally tied into your cloud-based EHR, you provide patients with the opportunity to learn more about your practice and their health at their convenience, whether that’s late in the evening or on a weekend. This type of access provides patients a sense of comfort because they know their records are always within reach, even when your office isn’t open or you’re not on call. Including some personally written content or material for patients to view and reference online will go a long way towards creating a helpful presence, while also reducing the amount of time you have to spend explaining that information.
Improve Communication
Similarly, many portals offer secure communication channels so patients can ask questions of you or your team. Have a plan in place to respond to these questions. Try to be as prompt as possible – within reason of course.
Some patient portals also allow for the ability to schedule – or at minimum request – appointments. By taking advantage of this feature, you can help eliminate lengthy wait times on the phone, which helps both your patients and your staff.
In return, you also have the ability to easily send patients appointment reminders or contact information when a patient needs their information for a referral.
Maintain Records
Allowing the patient to fill out forms in advance of appointments or update their own address and billing information and emergency contact list not only helps the patient get through the intake process more quickly, it helps your team become more efficient. In addition, many portals also offer patients the ability to pay outstanding balances through a secure payment system. In more complex patient portals, patients can update their prescription information and problem list to help physicians reduce the likelihood of adverse events.
Educate
Explaining esoteric health information like lab results over the phone, or even in person, can be an inefficient method for educating patients. Since the information is often unfamiliar, the chance they’ll forget the information or misplace their printed instructions can be high.
Through a patient portal, you can not only deliver test results that can be read at any time, you also have the opportunity to educate the patient and his family about what those results mean. Having a library of fact-based information regarding specific conditions or upcoming tests can help alleviate stress or confusion – and maybe even prevent the patient from conducting random searches online, finding inaccurate information, and arriving at ill-founded conclusions.
It’s also a great way to educate a patient about specialists or other doctors that you may be referring him to. While the patient portal system can be very disparate – different offices may or may not be using the same portal – you still have the ability to give a patient a basic fact sheet and office contact information for the referred doctor. This is yet another way to put a patient’s mind at ease.
more at http://healthworkscollective.com/zach-watson/177401/best-practices-boosting-patient-portal-engagement

|
Scooped by
nrip
|
Today in the highly digital world that we have come to live in, the experience has to be extended to the consumer’s devices: namely mobile phones, tablets and personal computers delivered on the backbone of the World Wide Web.
So in this era where consumers have come to expect more from their brands, are patients correct in demanding a better user experience from their care providers?
Healthcare organizations are aware of this expectation and they are also aware that physicians and their allied co-workers need a better medium to communicate and collaborate among them. This not only leads to a better experience for all but also is critical as hospitals continue to drive better clinical outcomes.
One of the aspects of digital engagement is providing an exceptional web experience, whether it is providing physicians with real time data and reports on the cases they are following or engaging patients with education that can help them manage their health better.
The digital experience can help in achieving the following
1) Provide a platform for better collaboration between physicians. Also this helps in increasing consultations between experts who are not necessarily collocated but still need a visual to make a better diagnosis.
2) Accentuates the sharing of information between hospitals and even between various departments of the same hospital.
3) Leveraging the existing hospital information to give a visual picture to the patients on education and how they can leverage the hospital and its facilities to the best of its ability.
4) Running extensive 360 degree programs involving various departments like surgery, nutrition and physiotherapy.
5) Providing a mechanism for better healthcare management.
scooped and summarized from http://insights-on-business.com/healthcare/healthcare-moving-towards-better-patient-experience-is-digital-the-answer/

|
Scooped by
nrip
|
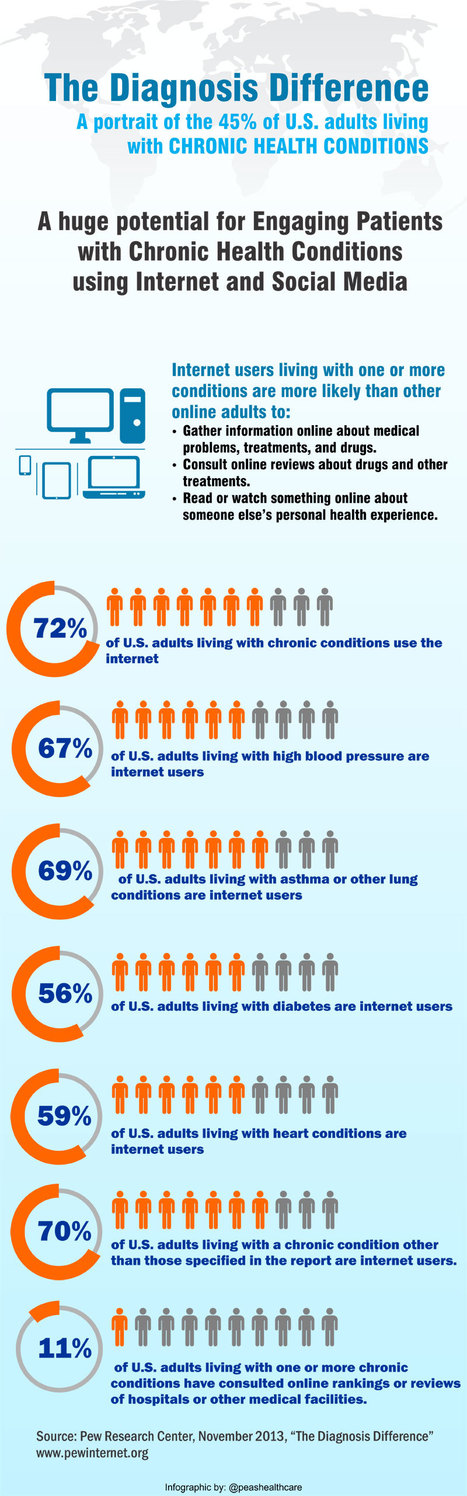
Patient engagement represents the next aim of healthcare reform through the adoption of health IT systems and services. It just received a boost from PCORI which awarded $93.5 million for the creation of 29 clinical research data networks that will combine to form its National Patient-Centered Clinical Research Network (PCORnet).
A major aim of establishing these networks is to enable the patient population to play an active role in how their care is delivered. “One of the reasons people think we should be engaging patients more actively is to make sure that as we do research we’re measuring and assessing the kinds of things they want to know when they’re making medical decisions,” says Elizabeth McGlynn, PhD, Director of the Center for Effectiveness & Safety Research at Kaiser Permanente.
“While we appreciate that more traditional biometric information may be important,” she continues, “there are a number of other things that any of us who have had to make decisions about whether or not to have a surgical procedure or take a particular drug would like to know beyond some of that information.” McGlynn and her team of researchers will rely on its network, Partners Patient Outcomes Research To Advance Learning (PORTAL), to change how a healthcare organization learns from its patients, namely in bridging the gap between the latter and researchers. “The whole area of engaging patients more actively and comprehensively in research is an evolving one.
At a high level, the challenges for the project are two-fold. On the one hand, researchers need to be able to understand how patients want to be engaged:
We know that patients aren’t homogenous; we know that there’s a range of opinion. These kinds of tools give us the chance to continue to appreciate the diversity of ideas and opinions and avoid trying to just get to the one or the two leading ideas but really to think. As people are exploring the notion of what personalized medicine means, how do we make sure that we’re eliciting information from people about what’s important to them personally?
On the other hand, they must tackle the challenge of making this feedback available to clinicians in a meaningful way:
One of our big challenges is finding ways to effectively integrate that information into the electronic health record. We have some work underway right now that’s given us some early insights into what patients are willing to provide if their doctors are going to see it and use it but if it’s just a hypothetical exercise, not so interested.
45% of U.S. adults live with chronic disease
Living with a chronic disease has an independent effect on people’s technology adoption and health behavior
72% of U.S. adults living with chronic conditions use the internet 7 in 10 track weight, diet, exercise routine, or symptoms 67% of U.S. adults living with high blood pressure are internet users
69% of U.S. adults living with asthma or other lung conditions are internet users
56% of U.S. adults living with diabetes are internet users
59% of U.S. adults living with heart conditions are internet users
70% of U.S. adults living with a chronic condition other than those specified in the report are internet users.
Surprisingly, only 11% of U.S. adults living with one or more chronic conditions have consulted online rankings or reviews of hospitals or other medical facilities.
People living with chronic conditions are more likely than others to fact check with a medical professional what they find online
The findings of this report presents a great opportunity of engaging patients with chronic conditions using internet and social media
Via Parag Vora
|



 Your new post is loading...
Your new post is loading...

























As we learn to live the after effects of the pandemic, even the skeptics have started agreeing that the future of care depends on hybrid models. A healthy mix of physical and tele(read virtual/remote) will be adopted - even by unwilling care providers as the consumers have clearly got a taste for it and liked it. And once we accept the hybrid model opening the doors for a accepted technology driven care process (unlike EHR's in 2010), the doors may widely open up further to allow Algorithmic analysis tools, screeners, diagostics to further add flavor to this mix.